Tag

Stroke
Created by: London Neurosurgery PartnershipDirectory:
Tags:
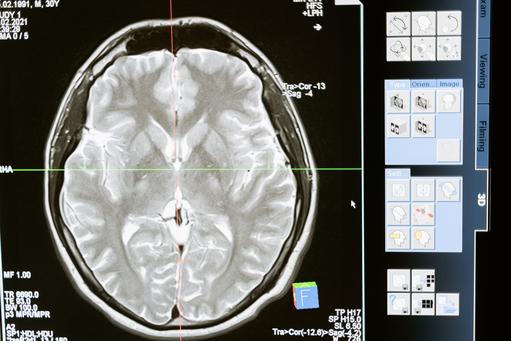
A Stroke is a sudden disruption of the blood supply of an area of the brain due to a blockage or narrowing of the arteries or bursting (bleeding) of one of the brain vessels.
go to clusterDirectory:
Tags:
Mr Tolias has been a Consultant Neurosurgeon at King’s College Hospital since September 2005. He has a PhD in Biological Sciences from the University of Warwick and extensive research experience in traumatic brain injury and the mechanisms of brain cell death. He undertook specialist training in neurosurgery in Liverpool and Birmingham followed by a Clinical Fellowship in Richmond, Virginia, USA. He is the Lead Neurovascular Surgeon at King’s College Hospital and the Associate Clinical Director for Trauma.
He is the first surgeon in the UK to perform the non-occlusive cerebral vascular bypass technique. In addition to his expertise in degenerative spine disease which includes the management of back and neck pain, arm pain and sciatica together with peripheral nerve disorders such as carpal tunnel syndrome; he has specialist expertise in the management of neurovascular conditions (e.g. cerebral aneurysms, AVMs, Cavernomas, AV fistulas), the surgical treatment of stroke (decompressive craniectomy and revascularisation for Moya-Moya, Sickle Cell Anaemia and trauma. His expertise extends to the use of radiosurgery (CyberKnife and GammaKnife) for the treatment of such conditions.

Christos Tolias
Consultant NeurosurgeonDirectory:
Expertise:
Mr Tolias has been a consultant Neurosurgeon at King’s College Hospital since September 2005.
He has a PhD in Biological Sciences from the University of Warwick and extensive research experience in traumatic brain injury.
Mr Tolias has vast Neurovascular experience and currently has the largest series of aneurysm surgeries in the UK (NNAP 2017).
He specialises in surgery of cerebral aneurysms, arteriovenous malformations, cavernomas and dural fistulas and rare conditions like Moya Moya.
He is one of the few surgeons in the UK who routinely performs cerebral vascular bypasses. He also performed the first ELANA bypass in the UK.
Mr Tolias has pioneered the use of bypass techniques in the management of cerebral vasculopathies.
He is trained in Gamma Knife and Cyberknife and routinely utilises innovative neuromonitoring technologies in the surgery of complex vascular lesions like arteriovenous malformations.
He is one of the few Neurosurgeons nationally who regularly undertakes surgical extirpation of arteriovenous malformations when indicated.
His outcomes are part of national databases and remain among the best in his peer group (NNAP 2017).
Alongside his subspecialty interest Mr Tolias has an active spinal practice dealing with problems of the cervical and lumbar spine. These can include sciatica, brachalgia, radiculopathies and pain management through both injections and radiofrequency ablation as well as surgical interventions.
Mr Tolias is the director of the first and only Royal College of Surgeons of England accredited National Neurovascular Surgical Fellowship based at King’s College Hospital.
He has over 60 papers in peer reviewed journals and more than 150 presentations at conferences. He regularly lectures in the UK and worldwide on topics including complex arteriovenous malformations, aneurysms, Gamma Knife and Cyberknife as well as degenerative spine conditions.
view this profile
Directory:
Expertise:
The London Neurosurgery Partnership is a unique concept in the provision of neurosurgical care. The team comprises eleven Consultant Neurosurgeons, all of whom are recognised superspecialists in their given area of expertise. As a result we can ensure that every patient seen by the group is matched with the Consultant Neurosurgeon best placed by virtue of their training and expertise to deliver the individualised and state of the art care each patient deserves.
Working as a team also ensures that our patients can access high quality neurosurgical care at all times from a consultant who will be familiar with their treatment plan at a location convenient to the patient. When appropriate, advice and treatment can be delivered by the composite team.
The London Neurosurgery Partnership has access to all of the latest neurosurgical technologies including the CyberKnife® and Gamma Knife® for radiosurgery which avoids the use of conventional open surgery in some cases and Minimally Invasive Techniques for both Cranial and Spinal neurosurgery when this is not possible. A key aspect of making use of such cutting edge technologies is the decision making process involved and this, in our opinion, is best done by a group of clinicians who are used to working together as a team to ensure that the latest technology and techniques are used appropriately based on the latest clinical guidelines.
view this profile
|
In January 2013 Andrew Marr, the 53-year-old BBC TV presenter and journalist, had a stroke after a bout of intensive exercise on a rowing machine in a gym. What is a stroke? A stroke is a serious medical emergency where the supply of blood to the brain is disrupted. In over 80% of cases, strokes usually happen because a blood clot blocks the blood supply to the brain. They can also happen when a weakened blood vessel that supplies the brain bursts and causes brain damage, known as a haemorrhagic stroke. Andrew Marr's stroke prompted two questions: (i) Do younger healthy people have strokes? and (ii) Does physical exercise contribute to strokes? Are stroke victims getting younger? Andrew Marr was one of 152,000 people in the UK who have strokes each year. Stroke is the third largest cause of death in the UK and the largest single cause of severe disability. There are approximately 1.1 million stroke survivors living in the UK and each year strokes cost the NHS £2.8 billion. The picture is no better in the US, where every 40 seconds a person has a stroke, each year strokes kill 130,000 and cost the US $38.6. Strokes are uncommon, but not rare in men in their fifties like Andrew Marr. Recent research suggests that strokes among the elderly are declining, while strokes among younger people are increasing. Between 1998 and 1999 in the UK, 9,000 people under 55 were admitted to hospital due to stroke. By 2011 this figure had risen to more than 1,600. It is not altogether clear why stroke is increasing among younger people, although experts note its correlation with type 2 diabetes. The importance of specialist stroke units Andrew Marr said that he believed what he read, that taking, "Very intensive exercise in short bursts is the way to health." Just before his stroke he said, "I went onto a rowing machine and gave it everything I had and had a strange feeling afterwards: a blinding headache and flashes of light". He took no notice and went home. The following morning he woke up lying on the floor unable to move. The most important care for people with any form of stroke is prompt admission to a specialist stroke unit, but even with prompt treatment a stroke can often be fatal. |
|
|




