Type-2 diabetes will not be prevented by repeating past failures
- England has embarked on a national diabetes prevention programme (DPP)
- In the UK, 64% of adults are classed as being overweight or obese
- Obesity is the main risk factor for type-2 diabetes
- Over the past decade diabetes in the UK has increased by 60% and now affects 4m
- Diabetes care consumes about 10% of the NHS’s annual budget of £116.4bn
- Traditional diabetes care and education fail to dent the UK’s diabetes burden
- The national DPP has got off to a slow start
- Type-2 diabetes will not be prevented by repeating past failures
- Lessons can be learnt from Oklahoma
Should we entrust an expensive national diabetes prevention programme to health officials who are failing?
DIABETES is a chronic disease, which occurs when the pancreas does not produce enough of the hormone insulin, or when the body cannot effectively use the insulin it produces. This leads to an increased concentration of glucose in the blood (hyperglycaemia). Type-1 diabetes is characterized by a lack of insulin production. Type-2 diabetes is caused by the body's ineffective use of insulin, and often results from excess body weight and physical inactivity
In the video below Sufyan Hussain describes type-2 diabetes; its propensity among certain ethnic groups, and some of its complications. Dr Hussain is a Darzi Fellow in Clinical Leadership, Specialist Registrar and Honorary Clinical Lecturer in Diabetes, Endocrinology and Metabolism at Imperial College Healthcare NHS Trust and Imperial College London. Also in the video are Richard Lane, former President of DUK who draws attention to pre-diabetes, and a patient with type-2 diabetes who describes his diagnosis and family history.

(click on the image to play)
The national diabetes prevention programme (DPP)
In March 2015 NHS England, Public Health England (PHE) and Diabetes UK (DUK) launched the NHS Diabetes Prevention Programme, (DPP), with the objective to limit the number of people developing type-2 diabetes. The DPP is an expensive national initiative expected to enrol up to five million people with blood sugar levels so high that they are at risk of the disease. See: Preventing diabetes in high-risk people.
“There are too many people on the cusp of developing type-2 diabetes, and we can change that. The growing body of evidence makes us confident that our national diabetes prevention programme will reduce the numbers of those at risk of going on to develop the debilitating disease,” says Professor Jonathan Valabhji, national clinical director for diabetes and obesity at NHS England, and one of the leaders of the DPP.
Eye-watering costs for failure
The UK’s record of diabetes care and prevention is poor. Despite £14bn being spent annually by the NHS on diabetes care, and some £20 million annually by DUK on diabetes education and awareness programmes, over the past 10 years people with diabetes have increased by 60%. Those responsible for diabetes care and support have not been held accountable, but continue to provide care and support that is failing to reduce the devastating personal, social and economic burden of diabetes. As a consequence the situation is becoming grave.
The latest figures from DUK suggest that the number of people with diabetes has topped four million - 8% of England’s adult population - and is on course to reach five million in less than a decade. In addition, there are currently 5 million people in England at high risk of developing type-2 diabetes. 64% of adults in the UK are either overweight or obese, which is the principal risk factor of type-2 diabetes. According to Professor Dame Sally Davies, the Chief Medical Officer, soaring rates of obesity pose such a threat that they should be treated as a “national risk” alongside terrorism.
If nothing changes, diabetes treatment costs alone could bankrupt the NHS. Despite these trends and the poor record of prevention and management, health officials leading the DPP confidently say that the new national programme will make a significant impact on the prevention of type-2 diabetes, and save £3 for every £1 spent. Officials however do not produce figures showing what the upfront costs of the programme will be.
Duncan Selbie, CEO of PHE and a leader of the DPP, said: “We know how to lower the risk of developing type-2 diabetes: lose weight, exercise and eat healthily . . . . PHE’s evidence review shows that supporting people along the way will help them protect their health, and that’s what our prevention programme will do.” In 2015-16, the DPP aims to support up to 10,000 people at risk of type-2 diabetes with “motivational coaches”, paid for by the NHS, to provide advice on weight loss, physical activity and diet.
The Public Accounts Committee takes up the cudgels
The Public Accounts Committee (PAC) has expressed serious criticisms of the way in which the DPP is setting about its task of limiting the number of people who develop type-2 diabetes.
It has said that the DPP is presenting an, "unduly healthy picture" of the state of diabetes services. "It’s not rocket science to tackle diabetes . . . . The NHS and Department for Health have been too slow in tackling diabetes, both in prevention and treatment . . . . . As a priority, action must be taken to ensure best practice in treatment and education is adopted across the board . . . . Taxpayers must have confidence that support is available when and where it is needed," says Meg Hillier, Chair of the PAC.
Not keeping pace
The PAC complained that the DPP’s approach lacked urgency, as some 200,000 people are newly diagnosed with diabetes every year, and it stressed that most people would be shocked to know that around 22,000 people with diabetes still die early every year.
Public Accounts Committee’s recommendations
The PAC said that the DPP, “will need to move at pace and at scale to stem the rising number of people with diabetes,” and recommended that by April 2016 the programme’s leaders, “set out a timetable to ramp up participation in the national DPP to 100,000 people a year, set out what it will cost, and how the programme will target those areas with the highest prevalence of diabetes. Public Health England should also set out how its other public health activities, such as marketing campaigns, will contribute to preventing diabetes.” The growing frustration of government officials with diabetes care and support is described in: Diabetes Wars
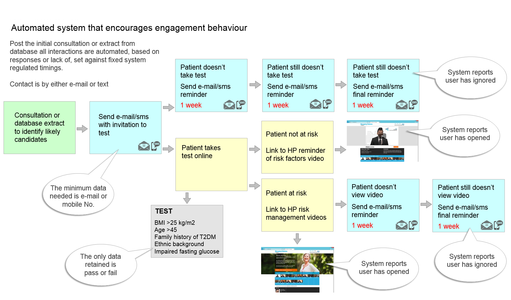
The PAC also expressed concerns about the low numbers of people either at risk of or living with diabetes who actually receive education to help them manage their condition. The committee recommended that the DPP, “develop a better and more flexible range of education support for diabetes patients.” Alternative diabetes educational programmes, which employ behavioural techniques to nudge people to change their diets and lifestyles, adhere to medication and get screened regularly, actually exist, but officials responsible for diabetes education turn a blind eye to these, and continue supporting traditional educational programmes that fail. See: Online video education can reduce the burden of diabetes and DUK and HealthPad agree on the importance of diabetes education
The Public Accounts Committee should demand more from the DPP
The PAC is right to recommend that the DPP “quickens its pace and increases its scope”; because, over the past 10 years, the NHS has spent more than £100bn on diabetes treatment alone, and DUK has spent some £200 million on education and awareness programmes, yet diabetes in the UK has increased by 60%.
Part of the responsibility for raising awareness and encouraging education among people living with diabetes falls to Diabetes UK, the largest and most influential charity for the condition in the UK. In addition to supporting research the charity is mandated to: (i) “Provide relief for people with diabetes and its related complications and to those who care for them, (ii) Promote the welfare of people with diabetes and its related complications and of those who care for them, and (iii) Advance the understanding of diabetes by education of people with diabetes, the health professionals and others who care for them, and the general public.”
Each year DUK spends about £20 million on, (i) raising awareness of diabetes, (ii) supporting self-management of the condition, and (iii) improving the quality of diabetes care. Despite this relatively large spend, DUK only manages to reach a relatively small percentage of the millions of people living with diabetes. For example in 2014, only 0.5% of people with diabetes used the DUK care line, the charity sent information packs to only 1.25% of the people with diabetes, only 0.3% signed up for e-learning courses, and only 0.4% of the 5 million people at risk of type-2 diabetes have used the DUK risk calculator.
The PAC is also right to demand more effective and flexible education programmes to propel people to self-manage their condition. Only 16% of people diagnosed with diabetes are offered traditional educational courses, and only 4% of these actually take up the courses. This suggests that there is a crying need for organizations responsible for diabetes education and awareness programmes to increase their understanding of how to engage people and nudge them to change their diets and lifestyles, and improve their use of online communications technology, which makes servicing any number of patient groups, of any size, in any geography, easy and cheap.
More importance should be given to patient outcomes
The PAC should demand more from the DPP, and recommend that it measures and reports annually on the programme’s success in preventing those at risk of type-2 diabetes from developing the condition. “I’ve been struck again and again by how important measurement is to improving the human condition. You can achieve amazing progress if you set a clear goal and find a measure that will drive progress toward that goal . . . This may seem pretty basic, but it’s amazing to me how often it is not done,” says Bill Gates. An earlier Commentary drew attention to the fact that UK diabetes agencies responsible for spending millions each year on diabetes education and awareness programmes which fail, only report on the distribution of services, rather than on the impact those services have had on patient outcomes, which is the most appropriate way of measuring the programme’s effectiveness. See, The importance of measuring the impact of diabetes care.
Oklahoma: America’s fattest city
Contrast England’s national DPP with an American prevention programme developed and led by Mike Cornett, the mayor of Oklahoma City, which is known as the “fattest city in America”. Cornett dealt with the challenge very differently.
Rejected doctors’ advice
Spurred on by his own weight-loss regime after discovering he was classed as obese, Mike Cornett wanted to transform Oklahoma City into a place where obesity could no longer thrive. While he was aware of the on going debates among clinicians and medical researchers about the best strategies to prevent type-2 diabetes, Cornett was not convinced that traditional health officials had credible answers. On New Year's Eve 2007, Cornett announced that Oklahoma City was going to go on a diet to lose a collective one million pounds.
Cornett did not start his prevention strategy by spending money to review evidence from existing diabetes studies; he did not develop a ‘framework’ to be reviewed and sanctioned by an expert panel of clinicians; he neither initiated primary care pilot projects, nor set up demonstrator sites in GPs’ surgeries; and he did not ask doctors to identify people with non-diabetic hyperglycaemia, defined as having an HbA1c of 42 – 47 mm/mol (6.0 – 6.4%) or a fasting plasma glucose (FPG) of 5.5 - 6.9 mmol/mol. In contrast, all the above was done by England’s DPP.
Losing one million pounds becomes a talking point
Having rejected the help of clinicians and healthcare officials, and without spending any money, Cornett started a website, thiscityisgoingonadiet.com, and encouraged citizens to register, and track how much weight they were losing.
His awareness campaign took off: churches set up running clubs, schools discussed diets, companies held contests to lose weight; restaurants competed to offer healthy meals. More importantly, people across the City began discussing obesity, which was a crisis spiralling out of control. More than 51,000 people, 59% of those over 45, signed up to his website and lost weight. By January 2012, Oklahoma City reached its target of shedding one million pounds.
Cornett was pleased that people had lost weight, but more importantly, he understood that the challenge was not over - it was just beginning. The hidden success of Cornett’s weight loss campaign was that he had successfully engaged an at-risk population. Obesity became a talking point. Mayor Cornett had successfully nudged a city population to change their diets and lifestyles and lose weight. “The message about nutrition and health penetrated Oklahoma City,” says Cornett.
Today, 30% of people in the central Oklahoma region, which includes Oklahoma City, are still obese. Oklahoma City’s obesity rates, while still rising, have been reduced from 6% to 1% a year. In the lowest income areas of the City, which have the highest rates of diabetes complications, key indicators of diabetes have been reduced by between 2% and 10% in five years, and the City overall has seen a 3% fall in diabetes related mortality rates.
“Changing the health of a community takes a long time - probably a generation,” says Cornett. On 7th April 2015, Oklahoma State introduced a law relating to diabetes prevention, which demanded “detailed action plans for battling diabetes with actionable items for consideration by the Legislature including, but not limited to, steps to reduce the impact of diabetes, pre-diabetes, and related diabetes complications.” This would not have happened had it not been for the actions and initiative taken by Mike Cornett.
Diabetes and the built environment
Now that a population was engaged, Cornett asked taxpayers for $777 million to fund projects designed to prevent type-2 diabetes in the long term by rebuilding Oklahoma City around the pedestrian rather than the car. The money was forthcoming and Cornett used it to change Oklahoma’s built environment by developing new parks, installing bicycle lanes, reducing driving lanes and introducing buses, creating a boating district, and building pavements, which had not been built for some 30 years. Recent years have seen growing research interest in the relationships between obesity and the built environment. Today, Oklahoma City is a real-time experiment for what happens when you alter the built environment that affects the way people live and behave.
Takeaways
Preventing type-2 diabetes will not be achieved by a group of academic clinicians and healthcare officials repeating past failures. Preventing type-2 diabetes entails winning the battle against obesity, reducing poverty, and changing peoples’ diets and lifestyles. To do this you first have to engage people and nudge them to change their behaviour.
If the Secretary of State for Health is serious about preventing type-2 diabetes in the UK he would do well to learn from what Mayor Cornett accomplished. Having done that, he should enlist the help of Mayor Boris Johnson to replace the current leaders of the national DPP.
|